Personalized Immune Cell Therapy Prolongs Survival and Improves Quality of Life in Lung Cancer Patients
Lung cancer is one of the highest cancer incidence and mortality worldwide, among which non-small cell lung cancer (NSCLC) accounts for ~85% and small cell lung cancer (SCLC) accounts for ~15%.
Traditional treatments such as surgery, chemotherapy, and radiotherapy have limited efficacy in patients with advanced lung cancer, with a 5-year survival rate less than 20%. In recent years, the development of immunotherapy has brought new hope to lung cancer patients, especially the combined applications developed by Shenzhen Geno-Immune Medical Institute (GIMI) including Engineered Immune Effector T cell (EIE) technology and Chimeric Antigen Receptor T cell (CAR-T) therapy, which has shown great potential to prolong survival and quality of life in patients.
Several cases of clinical applications of combined EIE and CAR-T therapy technologies in lung cancer from GIMI and collaboration hospitals are presented here [NCT03356808-Intervention of CAR-T against lung cancer, NCT03353428-Intervention of engineered immune effector cells against cancer, NCT03535246-Tumor associated antigen-specific engineered immune effector cells (EIE) against cancer].
Case Presentation
Case 1: Long-term remission in a patient with metastatic lung adenocarcinoma
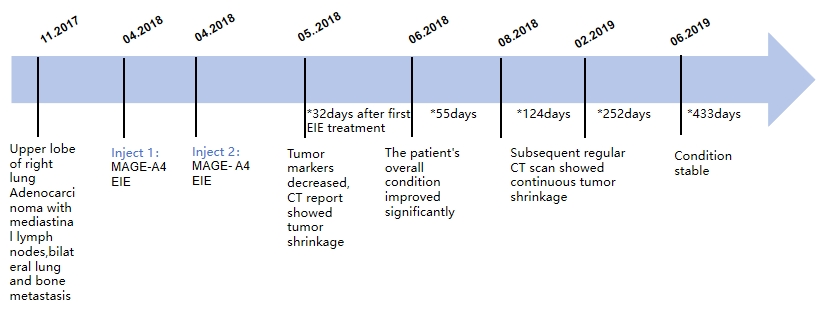
Patient information: A 55-year-old male, diagnosed with right upper lobe lung adenocarcinoma with mediastinal lymph node, bilateral lung, and bone metastases (cT2aN2M1a), inoperable.
Treatment Process:
-
Initial treatment: After diagnosis, the patient received 1 course of gemcitabine + cisplatin chemotherapy with no significant improvement; subsequent local radiotherapy was administered.
-
EIE treatment: Tumor puncture biopsy was obtained and precision immunohistochemical staining was done to screen for highly expressed target antigens, and MAGE-A4 was identified, and EIE cells were prepared. Radiotherapy was performed synchronously during the preparation period, and PD-1 antibody therapy was combined after EIE infusion.
-
Efficacy evaluation: Seven days after infusion, the patient felt numbness and pain in the lungs. One month later, tumor markers decreased, and CT showed tumor shrinkage. Fifty-five days later, the asthma symptoms disappeared, and subsequent regular CT examinations showed continuous tumor shrinkage, with stable condition for more than 3 years.
-
Mechanistic analysis: EIE cells recognized the tumor-specific antigen MAGE-A4, activated cytotoxic T lymphocytes (CTL), and directly killed tumor cells. Meanwhile, the combined applications of radiotherapy and PD-1 antibody might have reshaped the tumor microenvironment, enhanced immune cell infiltration and activity, which prevented tumor immune escape.
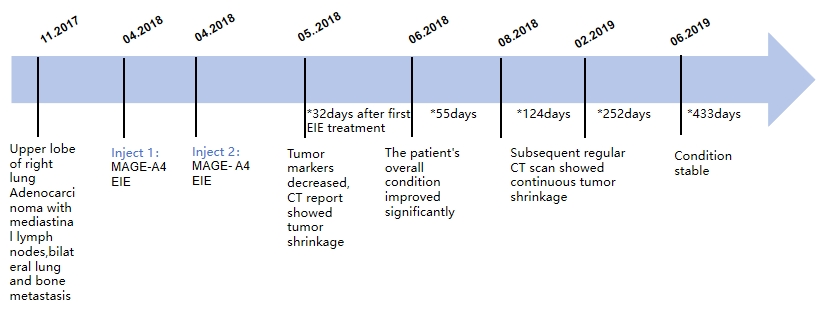
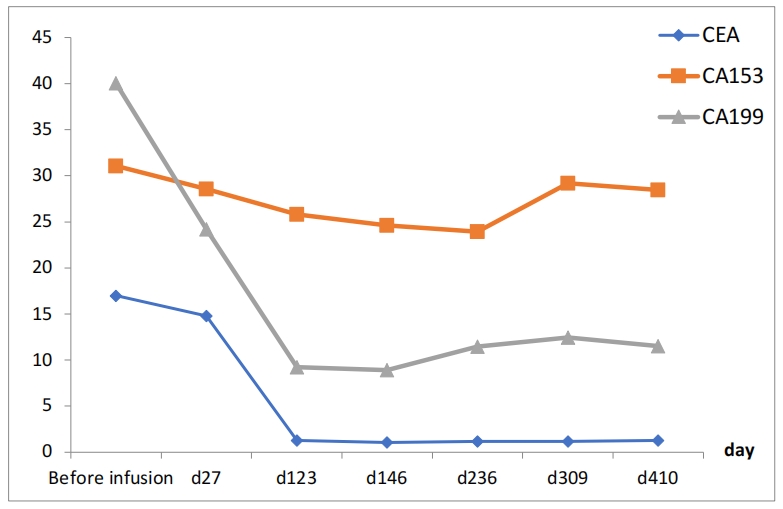
Figure 1: Treatment timeline and post-treatment tumor marker kinetics
Case 2: Stable control in a lung adenocarcinoma patient
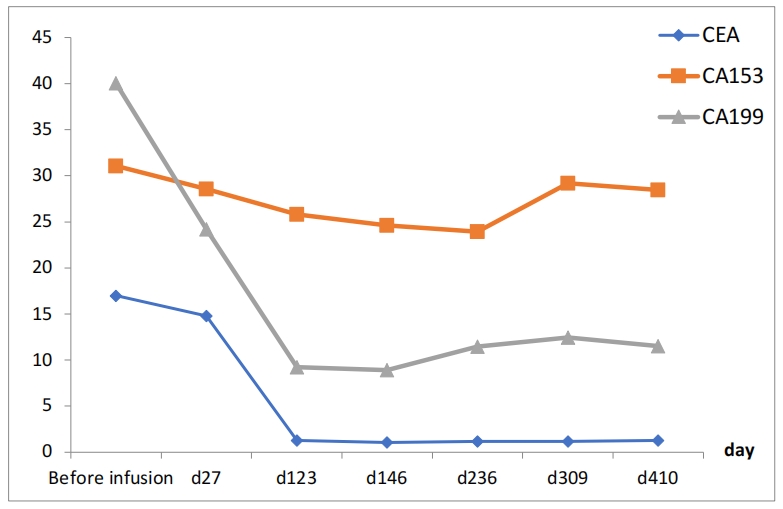
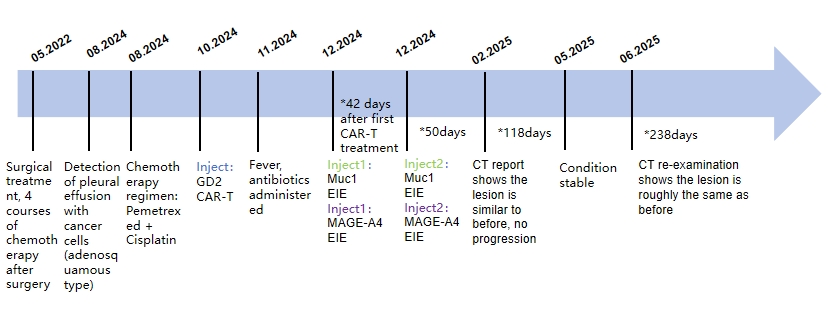
Patient information: A 44-year-old female, diagnosed with left lower lobe lung adenocarcinoma with multiple bone and pleural effusion metastases, stage IV.
Treatment process:
-
Initial treatment: 20 times of radiotherapy on 2 parts of the spine, 15 times of SBRT radiotherapy on the lung, and targeted drug administration during the period, but the treatment improvement was not significant, considering post-treatment changes of metastatic tumors.
-
CAR-T combined with EIE treatment: After precise immunohistochemical staining of the postoperative tumor to confirm the antigen targets, CAR-T cell therapy targeting Mesothelin antigen was adopted, and MUC-1 and MAGE-A3 were identified as additional targets to prepare EIE cells. The EIE cells were infused twice at short intervals about 1 month after CAR-T infusion.
-
Efficacy evaluation: About one week after CAR-T infusion, the patient developed asthma and dyspnea, which were relieved after 1 month. Then EIE combined therapy was performed. On the 62nd day after the immune cell therapy treatment, CT examination showed that the lesions were smaller than before, the left pleural effusion was reduced, and the condition has stabilized.
-
Mechanistic analysis: The 4sCAR modified T cells express CAR that recognizes Mesothelin. The CAR-T cells specifically bind to tumor cell surface antigens, activate T cell immune response, and directly kill tumor cells. MUC-1 is a cell surface antigen, and MAGE-A3 is an intracellular antigen. The dual combined targeting could cover different antigen presentation pathways and reduce tumor metastasis/immune escape.
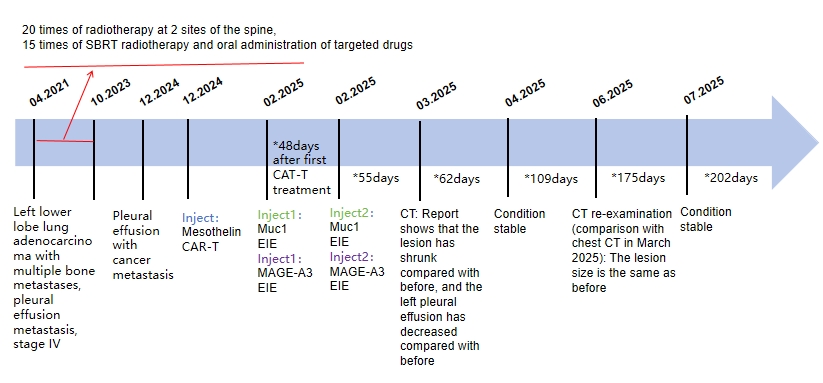
Figure 2: The timeline of CAR-T combined with EIE treatment
Case 3: Survival benefit in a patient with postoperative recurrence of lung cancer
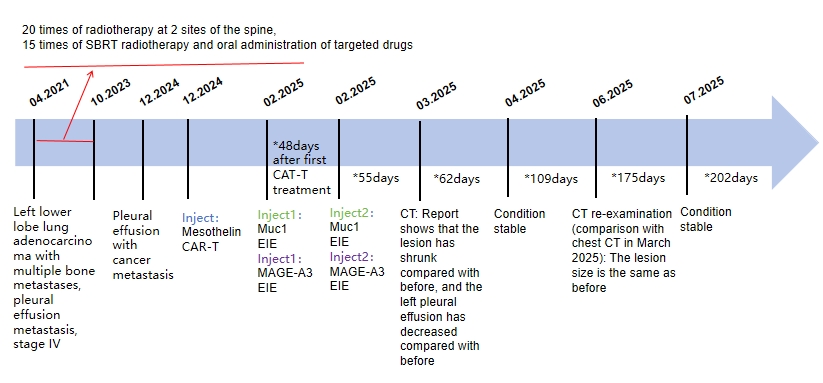
Patient information: A 63-year-old male, with postoperative recurrence of lung cancer (pleural effusion, mediastinal and hilar lymph nodes involvement).
Treatment process:
-
Initial treatment: Surgical treatment, 4 courses of chemotherapy after surgery, targeted drug administration after surgery, and pemetrexed + cisplatin chemotherapy.
-
CAR-T combined with EIE treatment: After immunohistochemical staining to confirm the antigen targets, CAR-T cell therapy targeting GD2 antigen was adopted, and MUC-1 + MAGE-A4 were identified as co-targets to prepare EIE cells. The EIE cells were infused twice at short intervals at 1 month after CAR-T infusion.
-
Efficacy evaluation: About one week after CAR-T infusion, the patient had a fever, which subsided after 1-2 days. The EIE treatment was performed one month later. After infusion, the patient had a fever, which returned to normal after 2-3 hours. On the 118th day after infusion, CT examination showed that the lesions were similar to before, and the condition was stable for more than half a year.
-
Mechanistic analysis: The CAR-T cells were prepared that recognized GD2 antigen, which could specifically bind to GD2-positive tumor cells, release cytokines and directly kill tumor cells. The MUC-1/MAGE-A4 targeting EIE enhanced CD8+ T cell immune response and reduced the invasion and metastasis ability of the tumor cells.
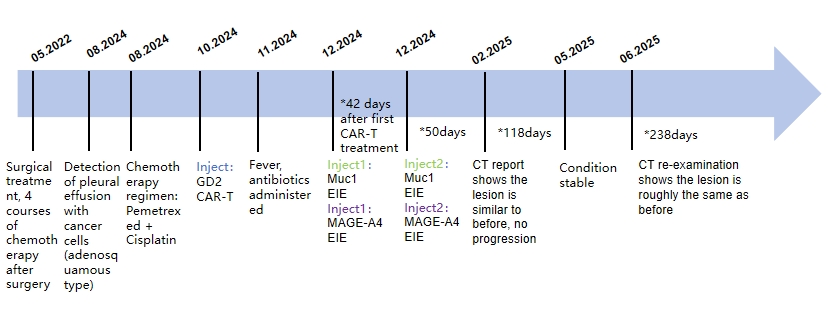
Figure 3: Timeline of CAR-T and EIE combination treatment
Conclusion
The innovative personalized EIE and CAR-T combined targeted immune cell therapy developed by GIMI has provided a new treatment option for advanced lung cancer patients. The targeted EIE cells can activate endogenous immune responses, kill tumors, and enhance the infiltration and activity of the CAR-T cells. The CAR-T cells can directly kill tumor cells, and the two together establish a synergistic effect. In cases of metastatic non-small cell lung cancer, this combined therapy strategy has shown a great potential to prolong survival and improve quality of life. For immune cell therapy of solid tumors, GIMI has carried out several innovative treatment schemes, and further improved the efficacy through individualized combination treatment strategies.